Whilst they’ve revolutionized the therapy of sure types of most cancers, CAR T-cell therapies have been shadowed by a major limitation: many sufferers, together with these whose most cancers goes into full remission, ultimately relapse. In a brand new research, Dana-Farber Most cancers Institute researchers report on a way with the potential to eradicate that drawback.
The method, described in a paper revealed on-line in the present day within the journal Nature Biotechnology, works by spurring CAR T cells to be extra energetic and persist longer within the physique, enabling them to stay in battle mode till all tumor cells are eradicated. The approach – creates what researchers dub a CAR-Enhancer (CAR-E) therapeutic platform – additionally causes CAR T cells to kind a reminiscence of the most cancers cell, to allow them to spring again into motion if the most cancers recurs.
In experiments in patient-derived laboratory most cancers cell strains and different research, CAR-Enhancer therapy succeeded in eradicating all tumor cells, clearing the way in which for medical trials of this method in human sufferers. Researchers hope to launch the primary trial within the close to future.
“CAR T-cell therapies have been a breakthrough therapy for B-cell hematologic cancers akin to B-cell leukemias and lymphomas and a number of myeloma,” says the research’s senior creator, Mohammad Rashidian, PhD, of Dana-Farber.
In myeloma, for instance, just about one hundred pc of sufferers have a superb response to CAR T-cell therapies initially, however nearly all relapse, half of them inside one to 2 years of therapy. Relapse coincides with the disappearance of CAR T-cells within the bloodstream.”
Mohammad Rashidian, Dana-Farber Most cancers Institute
“Many of the analysis to deal with this problem has centered on re-engineering the CAR T cell itself – for instance, by introducing or eliminating genes to maintain the cell energetic for longer,” he continues. “Whereas these approaches maintain nice promise, they’ve but to indicate a lot effectiveness within the clinic. We determined to return on the drawback from a totally totally different perspective.”
As a substitute of making an attempt to change the internal workings of CAR T cells, Rashidian and his colleagues developed an method that works from the skin – by delivering to the cells’ doorstep a molecule that extends their lives and prompts them to kind reminiscence. The automobile for carrying out this can be a fused-together “platform” not like another utilized in medical therapy.
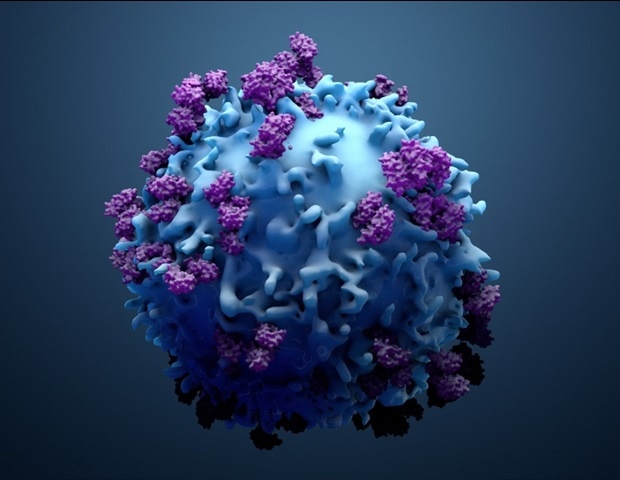
CAR T cells are genetically enhanced variations of a affected person’s personal cancer-fighting T cells. They’re made by eradicating a couple of million T cells from a affected person’s blood and genetically equipping them to provide a particular construction, known as a chimeric antigen receptor, or CAR, on their floor. The CAR is designed to latch onto a particular marker, or antigen, on a affected person’s tumor cells. The cells, now known as CAR T cells, are grown in a lab till they quantity within the tons of of hundreds of thousands. When the cells are infused again into the affected person, their specifically designed receptor locks onto the tumor cell antigen and triggers an immune system assault on the most cancers.
“The assault destroys almost all of the tumor cells, however a tiny share stays,” Rashidian explains. “The CAR T cells are effector cells: they stay to kill most cancers cells. Once they cannot discover any extra to kill, they act as if their job is finished and go away. The remaining tumor cells, nonetheless, can set the stage for a resurgence of the most cancers.”
To delay the CAR T cells’ assault and endow them with reminiscence, the Dana-Farber researchers developed a totally novel therapeutic agent, the CAR-E platform. It consists of a weakened type of the immune-signaling molecule interleukin-2 (IL-2) fused to the very antigen the CAR is designed to bind to.
“IL-2 has a powerful impact on T cells – activating them and inflicting them to proliferate – nevertheless it may also be extremely poisonous to sufferers,” Rashidian remarks. “For that motive, we used a really weak type of it. By itself, it has no impact on regular T cells however has a stimulatory impact on CAR T cells when focused particularly to them.”
That precision concentrating on is completed by fusing IL-2 to a particular antigen. In CAR T-cell therapies for a number of myeloma, the CAR binds to an antigen known as B-cell maturation antigen (BCMA) on myeloma cells. It’s that antigen that’s affixed to IL-2 within the new remedy.
“Identical to weak IL-2, the BCMA antigen by itself would not have an effect on CAR T cells, however, collectively, they’ve a synergy whose impression was properly past our expectations,” says the research’s first creator Taha Rakhshandehroo, PhD, of Dana-Farber.
CAR-E remedy not solely causes CAR T cells to proliferate however to diversify – to generate various kinds of CAR T cells with totally different properties – researchers discovered. “It generated not solely effector T cells, which most sufferers have already got, but additionally stem cell-like reminiscence T cells, central reminiscence T cells, effector reminiscence T cells – a whole repertoire of the sorts of T cells wanted for an efficient immune response to most cancers,” Rashidian remarks.
In laboratory cultures of myeloma cells and in animal fashions of the illness, CAR-E remedy introduced concerning the full clearance of tumor cells – an erasure of any signal of the most cancers – researchers discovered.
There have been different advantages as properly. Researchers found that the long-lasting CAR T cells generated by the remedy could possibly be re-stimulated by re-administering CAR-E. This implies that sufferers who relapse after CAR T-cell remedy could possibly be successfully handled with further doses of CAR-E therapy. CAR-E additionally raises that chance that sufferers could possibly be handled with smaller numbers of CAR T cells than at current. The present apply of permitting CAR T cells to multiply into the tons of of hundreds of thousands is a time-consuming, costly, resource-heavy course of that requires sufferers to attend many weeks earlier than receiving an infusion of the cells. The massive portions are partly answerable for some of the widespread negative effects of CAR T-cell remedy: cytokine launch syndrome, wherein an over-aggressive immune response ends in fever, nausea, speedy heartbeat, neurological issues or different points. With CAR-E, it could be potential to skip the CAR T-cell enlargement course of altogether: CAR T cells would merely be made and infused into sufferers, adopted by therapy with CAR-E.
“In animal research, we infused mice with very low numbers of CAR T cells and located that weren’t in a position to clear the most cancers,” Rashidian relates. “After we gave them the CAR-E therapy, the CAR T cells expanded and have been in a position to clear the most cancers.”
One of many first objectives of a medical trial of CAR-E remedy can be to make sure security and to find out the most effective dose and schedule of administration. Initially, they count on that the therapy would start a couple of month after sufferers are infused with CAR T cells. Therapy would encompass a weekly dose of CAR-E remedy for 3 or 4 weeks.
“Probably the most thrilling a part of this remedy is how simply it may be built-in into the care of sufferers receiving CAR T-cell therapies,” Rakhshandehroo says. “It is such a chic resolution to the issue of CAR T-cell depletion. We’re keen to start testing it in medical trials.”
